1. Introduction
The discovery and development of new drugs remain among the most complex and resource-intensive endeavors in biomedical science. On average, it takes between 12 and 15 years and over $2.6 billion USD to bring a single new drug to market, with attrition rates in clinical development stages exceeding 90% (DiMasi, Grabowski, & Hansen, 2016; Wouters, McKee, & Luyten, 2020). These failures are often due to inadequate efficacy, unforeseen toxicity, poor pharmacokinetics, or commercial considerations that become apparent only in late-stage trials. As a result, there is a growing interest in more efficient strategies such as drug repurposing to mitigate these challenges and expedite therapeutic innovation.
The rising global disease burden is driven by cancer, metabolic disorders, and chronic inflammation, all of which are closely linked to oxidative stress (Omiyale et al., 2024a). This imbalance in reactive oxygen species contributes to disease progression and is often worsened by exposure to environmental toxicants. Cancer arises from genetic and epigenetic changes that enable uncontrolled growth and therapy resistance. Natural products, with their antioxidant and anti-inflammatory properties, offer therapeutic promise, while drug repurposing provides a cost-effective way to target complex diseases (Ogunlakin et al., 2025a). Combining these approaches could lead to innovative, multi-targeted treatments for chronic and malignant conditions.
Drug repurposing, also known as drug repositioning or reprofiling, refers to the process of identifying new therapeutic indications for existing drugs, including those already approved, previously shelved due to non-safety reasons, or currently undergoing investigation for different diseases (Pushpakom et al., 2019). This approach capitalizes on existing data related to a drug’s safety, pharmacodynamics, pharmacokinetics, and manufacturing processes, thereby substantially reducing the time, cost, and risk associated with drug development. Unlike traditional pipelines that begin with novel compounds and untested mechanisms, repurposing allows for an accelerated bench-to-bedside trajectory. Furthermore, the method is applicable across molecular classes—ranging from small molecules and biologics to phytochemicals and even traditional medicines—and may be guided by target-based, phenotype-driven, or disease-similarity frameworks (Parvathaneni & Gupta, 2020).
Drug repurposing has yielded key therapies, such as thalidomide for multiple myeloma (Singhal et al., 1999) and sildenafil for erectile dysfunction and pulmonary hypertension (Ghofrani et al., 2006). Once driven by clinical observation, repurposing is now guided by computational tools like CMap, DrugBank, and AI models that analyze drug-disease molecular profiles (Lamb et al., 2006; Zhou et al., 2020). Additionally, real-world data from electronic health records have identified new uses for drugs like statins and SSRIs (Nielsen et al., 2012; Wang et al., 2014), with modern analytical methods enhancing the reliability of these findings (Hernán & Robins, 2016).
Drug repurposing has proven crucial during public health emergencies, notably in the COVID-19 pandemic, where drugs like remdesivir and dexamethasone were rapidly deployed based on known mechanisms and safety (Beigel et al., 2020; RECOVERY Collaborative Group, 2021). While some candidates like hydroxychloroquine failed under clinical testing (Borba et al., 2020), these efforts underscored the value of leveraging existing drugs
Repurposing also offers vital opportunities for non-communicable diseases and neglected conditions where drug development incentives are limited (WHO, 2023; Yin, 2008). However, challenges include intellectual property barriers, regulatory hurdles, limited financial returns, and ethical issues related to off-label use without strong evidence (Nosengo, 2016). Thorough mechanistic and clinical validation remains essential.
This systematic review aims to synthesize and critically evaluate the evolving landscape of drug repurposing. Specifically, we examine its historical development, mechanistic foundations, computational and experimental methodologies, real-world applications, regulatory considerations, and associated challenges. By highlighting successful case studies and identifying emerging technologies—such as AI-guided repositioning, multi-omics integration, and global open-science platforms—we provide a roadmap for translating repurposing discoveries into clinical impact. In doing so, we underscore the urgency and feasibility of repositioning existing pharmacological assets to address unmet medical needs and improve global health outcomes.
2. Methodology
2.1 Search Strategy
A comprehensive literature search was performed using five major electronic databases: PubMed, Embase, Web of Science, Scopus, and ClinicalTrials.gov. These databases were selected to ensure coverage of both biomedical research and clinical trials. The search strategy incorporated both controlled vocabulary (e.g., MeSH terms) and free-text keywords, linked using Boolean operators. The primary search terms included “drug repurposing,” “drug repositioning,” “drug reprofiling,” and “therapeutic switching.” These were further refined by pairing them with thematic qualifiers such as “mechanism,” “computational,” “regulatory,” “success stories,” and “clinical application.” Searches were limited to English-language articles published between January 2000 and June 2025 to capture contemporary developments in drug repurposing. To enhance the breadth of the review, additional sources were located using Google Scholar and through backward and forward reference chaining, consistent with best practices in systematic review methodology (Haddaway et al., 2015).
2.2 Inclusion and Exclusion Criteria
Studies were included in the review if they met several essential criteria. First, each article had to focus on mechanisms, strategies, or real-world applications of drug repurposing. Second, the study design needed to be methodologically robust, encompassing original research, systematic reviews, or meta-analyses. Third, included studies had to engage with at least one of the following domains: regulatory or ethical considerations, clinical implementation, or technological frameworks relevant to drug repositioning. Articles were excluded if they focused exclusively on in vitro experiments or non-translational animal studies that lacked a clear clinical bridge. Additional exclusions were applied to editorial commentaries, opinion pieces lacking empirical data, and publications not available in English. These criteria were aligned with the Cochrane Handbook’s recommendations for ensuring relevance and minimizing bias in systematic reviews (Higgins et al., 2022).
2.3 Data Extraction and Quality Assessment
Data from eligible studies were systematically extracted using a standardized data abstraction form developed in Microsoft Excel. Information collected included bibliographic details, study type, therapeutic focus, drug class, repurposing strategy, reported clinical or mechanistic outcomes, and study limitations. Each article was reviewed independently by two trained investigators to ensure consistency in data collection and interpretation. In instances where discrepancies arose, consensus was reached through discussion or consultation with a third reviewer. Quality assessment was carried out using the Joanna Briggs Institute (JBI) critical appraisal tools, which are tailored to assess methodological quality across different study designs (Munn et al., 2020). Each study was rated as high, moderate, or low quality based on the clarity of its aims, appropriateness of methodology, reliability of outcome measurement, and generalizability of findings. Only studies with sufficient methodological clarity and relevance were retained for final synthesis.
2.4 PRISMA Flow Diagram
The literature search and screening process adhered to the PRISMA 2020 guidelines (Page et al., 2021) and is visually summarized in a corresponding flow diagram. Records were systematically identified from multiple sources, and duplicates were removed prior to screening. Titles and abstracts were then assessed for relevance, with a subset of articles selected for full-text review. After applying predefined inclusion and exclusion criteria, a final group of studies was included in the synthesis. Articles were excluded for reasons such as lack of relevance to drug repurposing, absence of clinical or translational focus, redundancy, or language limitations. The included studies represented a diverse mix of methodologies, including observational research, randomized trials, computational modeling, and regulatory-focused analyses.
3.0 Integrative Approaches to the Burden of Chronic Diseases: Roles of Oxidative Stress, Toxicants, Natural Products, and Drug Repurposing
The global burden of disease is increasingly dominated by chronic non-communicable disorders, particularly cancer, metabolic diseases such as diabetes and obesity, and chronic inflammatory conditions. These diseases are major contributors to morbidity and mortality worldwide and account for over 70% of all deaths globally, with cancer alone responsible for approximately 10 million deaths annually (WHO, 2023). Urbanization, sedentary lifestyles, dietary changes, and aging populations have accelerated the prevalence of these conditions, especially in low- and middle-income countries (GBD 2019 Risk Factors Collaborators, 2020).
A unifying pathogenic mechanism across many of these chronic conditions is oxidative stress, defined as an imbalance between the production of reactive oxygen species (ROS) and the antioxidant defense system. Excess ROS leads to oxidative damage to cellular lipids, proteins, and nucleic acids, contributing to the initiation and progression of metabolic dysfunction, atherosclerosis, neurodegeneration, and tumorigenesis (Sies et al., 2017). Inflammation and oxidative stress are closely intertwined; chronic inflammation generates ROS, which in turn amplify pro-inflammatory pathways such as NF-κB, forming a vicious cycle that sustains tissue damage and disease progression (Reuter et al., 2010). Environmental toxicants play a significant role in the etiology of many chronic diseases. Exposure to heavy metals like cadmium and arsenic, air pollutants, pesticides, and endocrine-disrupting chemicals (EDCs) has been linked to metabolic disorders, immune dysfunction, and carcinogenesis (Klaunig, 2018; Heindel et al., 2017; (Onah et al., 2024; Edema et al., 2023; Ogunjobi et al., 2025; Omiyale et al., 2024b). These toxicants can induce DNA damage, epigenetic modifications, and disruption of cellular signaling pathways. Persistent organic pollutants and industrial chemicals have been shown to promote oxidative stress and interfere with hormone function, contributing to obesity, insulin resistance, and reproductive cancers (Jin et al., 2021).
Cancer development is a complex multistep process involving the accumulation of genetic mutations, epigenetic changes, and alterations in the tumor microenvironment. Chronic inflammation and oxidative stress contribute to every stage of tumorigenesis—from initiation through promotion to progression—by fostering genomic instability, immune evasion, and angiogenesis (Colotta et al., 2009). Tumor-associated macrophages, cytokines, and inflammatory mediators help remodel the microenvironment to favor cancer cell survival and metastasis.
In this context, natural products have received renewed attention for their therapeutic potential. Many bioactive compounds derived from plants, microbes, and marine organisms possess antioxidant, anti-inflammatory (Ogunlakin et al., 2025b), and anti-cancer properties (Atanasov et al., 2021; Oluyemis et al., 2021; Adegbesan et al., 2021; Ogunlabi et al., 2020; Ogunlakin et al., 2024; Ogunlakin et al., 2025c). Agents such as curcumin, resveratrol, and quercetin modulate multiple signaling pathways involved in apoptosis, angiogenesis, and immune modulation, making them promising candidates for both prevention and therapy in cancer and metabolic diseases (Newman & Cragg, 2020).
Alongside natural products, drug repurposing—the use of existing drugs for new therapeutic indications—offers a time- and cost-efficient strategy to accelerate treatment options for chronic diseases. Repurposed drugs like metformin (originally for diabetes, now studied in cancer and aging) and thalidomide (from sedative to anti-myeloma agent) illustrate the power of this approach (Pushpakom et al., 2019). Repurposing is particularly valuable in oncology and immunometabolic disorders, where drug development pipelines are long and failure rates are high. When combined with natural compounds, repurposed drugs may act synergistically to enhance efficacy and reduce toxicity.
In conclusion, the growing burden of chronic diseases demands integrative therapeutic strategies that address underlying mechanisms such as oxidative stress, inflammation, and toxicant exposure. The convergence of natural product discovery and drug repurposing offers a promising path toward safer, multitargeted, and cost-effective treatments for cancer and other chronic conditions.
4. Mechanisms and Rationale for Drug Repurposing
Drug repurposing draws on a diverse range of biological, pharmacological, and computational insights to identify new therapeutic indications for existing pharmaceutical compounds. As modern pharmacology evolves beyond the “one drug, one target” paradigm, it has become evident that many compounds exert effects on multiple biological systems, offering new opportunities for intervention in diseases outside their original indication (Ashburn & Thor, 2004; Nosengo, 2016). These opportunities are often discovered through mechanisms broadly categorized into three interrelated frameworks: target-based repurposing, disease-based repurposing, and phenotypic or signature-based screening. Each of these approaches is supported by advances in omics technologies, systems pharmacology, and artificial intelligence, allowing for more precise and rational repositioning strategies.
4.1 Target-Based Repurposing
Target-based repurposing focuses on identifying shared or analogous molecular targets—such as receptors, enzymes, transporters, or kinases—that are implicated in more than one disease. If a drug effectively binds and modulates a particular protein in one indication, it may exert therapeutic benefits in another condition where the same or a similar target plays a pathogenic role. This approach benefits from advances in structural bioinformatics, which enable comparative analyses of drug-target interactions across different disease contexts.
A landmark example is imatinib mesylate, initially approved for the treatment of chronic myeloid leukemia (CML) due to its inhibition of the BCR-ABL fusion tyrosine kinase. Later research demonstrated that imatinib also inhibits the receptor tyrosine kinase c-KIT, which is constitutively activated in gastrointestinal stromal tumors (GISTs)—leading to its FDA approval for this second indication (Demetri et al., 2002). This case illustrates how understanding target homology and molecular docking characteristics can inform repurposing decisions.
High-resolution protein structural data and computational docking simulations now allow researchers to assess whether a drug developed for one target can bind to similar active sites in other proteins. Moreover, network pharmacology models have revealed that many diseases share key nodal proteins within biological interaction networks, particularly in inflammatory, oncogenic, and fibrotic pathways (Zhou, Wang, & Cheng, 2015; Guney & Oliva, 2012). For example, shared pro-inflammatory targets like NF-κB or TNF-α are implicated in cancer, autoimmune diseases, and neurodegeneration, supporting the rationale for cross-disease therapeutic strategies.
4.2 Disease-Based Repurposing
Unlike the target-centric model, disease-based repurposing focuses on pathophysiological similarities between diseases, rather than shared targets. In this framework, drugs may be repositioned based on the observation that two or more diseases involve similar immune responses, metabolic dysfunction, genetic profiles, or tissue pathologies. By intervening in common mechanisms, a drug may provide benefit across multiple indications even without a shared molecular target.
A well-established example is the use of adalimumab, a TNF-α inhibitor originally developed for rheumatoid arthritis, in the treatment of inflammatory bowel disease (IBD). Although the diseases affect different organ systems—joints versus the gastrointestinal tract—both involve dysregulated TNF-α signaling, and the efficacy of adalimumab in Crohn’s disease and ulcerative colitis has been demonstrated through numerous clinical trials (Sandborn et al., 2007).
Advancements in disease-disease network modeling have greatly enhanced this strategy. By integrating transcriptomic data from disease samples, researchers can generate similarity scores between diseases and construct interaction networks to prioritize shared biological processes. This systems-level view enables the identification of novel therapeutic applications for drugs by revealing molecular convergence points between seemingly unrelated conditions (Himmelstein et al., 2017; Dudley, Deshpande, & Butte, 2011).
For instance, transcriptome-wide analysis has revealed similarities in inflammatory gene expression between psoriasis and atherosclerosis, leading to exploration of anti-inflammatory agents originally developed for skin diseases in cardiovascular contexts (Ritchie et al., 2015). Such computational methods are particularly useful for diseases with complex or poorly defined etiologies, such as Alzheimer’s disease and systemic lupus erythematosus.
4.3 Phenotypic and Signature-Based Screening
Phenotypic repurposing refers to the identification of new indications based on observable biological responses in preclinical or clinical models. This strategy does not rely on pre-specified molecular targets but instead evaluates a drug’s ability to induce a desired phenotype, such as reduced tumor growth, improved neuronal survival, or behavioral changes in animal models. Phenotypic screening was historically the dominant method for drug discovery and is regaining importance with the emergence of high-throughput and high-content screening technologies.
Modern adaptations of this approach use transcriptomic signatures and other omics data to associate drugs with diseases based on pattern reversal or similarity. A key development in this area is the Connectivity Map (CMap), which correlates the gene expression profiles of disease states with drug-induced transcriptional changes. Drugs that reverse the disease-specific expression pattern are hypothesized to have therapeutic potential (Lamb et al., 2006). This strategy has facilitated the identification of repositioning candidates across multiple indications, including oncology, infectious diseases, and psychiatric disorders.
An illustrative case is the repositioning of topiramate, an antiepileptic drug, for binge eating disorder (BED). Initially approved for seizure control, topiramate was observed to influence appetite and impulsivity in both preclinical models and human trials. Follow-up studies confirmed its efficacy in reducing binge episodes, leading to its off-label use and further investigation in obesity-related disorders (McElroy et al., 2003; Guerdjikova et al., 2005).
Phenotypic screening is also useful for identifying multi-target or “dirty” drugs that act on several pathways simultaneously—a common feature of effective agents for complex disorders like cancer and neuropsychiatric conditions. Furthermore, integrating transcriptomic data with machine learning tools has enabled the rapid prediction of candidate compounds that may normalize disease-associated signatures. This integration of artificial intelligence with biological profiling is expected to play a transformative role in future repurposing efforts (Aliper et al., 2016; Peón et al., 2021).
In conclusion, the mechanistic rationale behind drug repurposing is multifaceted and increasingly informed by systems biology, omics data, and computational modeling. Whether grounded in target homology, disease similarity, or transcriptional modulation, these approaches provide a powerful foundation for discovering novel therapeutic uses for existing compounds. As the scope and precision of biomedical data continue to expand, these mechanistic strategies will play a central role in accelerating innovation in drug development.
5. Drug Repurposing Strategies
Over the past two decades, drug repurposing has evolved from an opportunistic, serendipitous process to a systematic and data-driven endeavor. Earlier repositioning efforts often relied on chance clinical observations or anecdotal reports of off-target therapeutic effects. However, with the advent of high-throughput molecular technologies, advanced computational modeling, and real-world data integration, repurposing strategies now span a wide methodological spectrum. These include computational prediction models, phenotypic high-throughput screening, multi-omics integration, and the mining of electronic health records. Each approach contributes uniquely to the expanding toolkit of modern drug repositioning.
5.1 Computational Approaches
One of the most transformative developments in the field has been the emergence of computational strategies that leverage big data to predict novel drug-disease associations. These techniques encompass network-based pharmacology, molecular docking, and artificial intelligence-driven learning models.
5.2 Network-Based Pharmacology
Network pharmacology conceptualizes biological systems as complex, interconnected networks where nodes represent biological entities such as genes, proteins, or pathways, and edges represent functional or regulatory relationships. In this framework, disease modules are often embedded within larger interactomes, and drugs can be viewed as perturbations targeting specific nodes or modules. Repurposing strategies based on this concept aim to identify key “hub” proteins or shared pathways that link multiple diseases (Barabási et al., 2011).
Algorithms like Random Walk with Restart (RWR), DeepDTnet, and DrugNet use graph theory and machine learning to traverse protein-protein interaction networks and prioritize drug-disease relationships. These tools compute proximity scores between drug targets and disease-associated modules, enabling the identification of repositioning candidates that affect multiple pathological processes simultaneously (Zhou et al., 2020). Such methods have been particularly impactful in complex diseases like cancer and neurodegeneration, where polygenic and network-level dysregulation is common.
5.3 Molecular Docking and Structural Similarity
Structure-based drug repurposing relies on in silico molecular docking, a computational technique that simulates the interaction between small molecules and target proteins. This approach evaluates the binding affinity of compounds to active sites of disease-relevant proteins by modeling receptor-ligand interactions in three dimensions. Through virtual screening, thousands of FDA-approved or investigational compounds can be tested against a protein target in a matter of hours, identifying promising binders for further validation (Pagadala, Syed, & Tuszynski, 2017).
During the COVID-19 pandemic, molecular docking was extensively used to screen for inhibitors of the SARS-CoV-2 main protease and spike protein. For example, Ton et al. (2020) applied deep docking techniques to screen over one billion compounds and identified multiple repurposing candidates for COVID-19, including kinase inhibitors and antiviral agents. In parallel, ligand-based virtual screening, which relies on molecular fingerprint similarity rather than explicit docking, has proven valuable in identifying analogs of known active compounds that may function in new therapeutic contexts (Cherkasov et al., 2014).
5.4 Machine Learning and Artificial Intelligence
Artificial intelligence (AI) and machine learning (ML) models have revolutionized the drug repurposing landscape by enabling pattern recognition across diverse biomedical datasets. These models are trained on large-scale gene expression profiles, drug-target interactions, chemical structures, and clinical outcome data to identify latent associations between drugs and diseases that may not be obvious through conventional methods.
Platforms such as DeepChem, PharmAI, and RepurposeDB integrate transcriptomic and cheminformatic data using deep learning algorithms to predict therapeutic repositioning opportunities. Aliper et al. (2016) demonstrated that deep neural networks trained on gene expression signatures could accurately classify pharmacological properties and predict new indications for existing drugs. AI models further benefit from iterative learning and can be adapted to rapidly evolving therapeutic landscapes, such as emerging cancer subtypes or viral variants, through reinforcement learning frameworks. These tools are particularly suited to identifying multitarget agents and repurposing in polygenic disorders where network-based and single-target models may fall short.
5.5 High-Throughput Screening (HTS)
While computational methods offer powerful predictions, experimental validation remains critical. High-throughput screening (HTS) continues to play a foundational role in empirical drug repurposing, particularly through phenotypic assays that assess compound effects on cellular or organismal models. HTS platforms are capable of evaluating thousands of chemical entities in a single experiment, providing a rapid means of identifying previously unrecognized bioactivities. Drug libraries such as the Prestwick Chemical Library, NIH Clinical Collection, and ReFRAME contain thousands of clinically approved, investigational, or withdrawn drugs curated for repurposing potential (Janiszewski, 2020). For example, niclosamide, a well-known antiparasitic agent, was identified via HTS as a potent inhibitor of the Wnt/β-catenin signaling pathway in prostate cancer models. Osada et al. (2011) demonstrated that niclosamide suppressed tumor growth and metastasis in preclinical systems, prompting its investigation in cancer clinical trials.
Similarly, itraconazole, an antifungal agent, was repositioned as a Hedgehog pathway inhibitor through HTS, exhibiting antiangiogenic and anticancer effects in basal cell carcinoma and non-small-cell lung cancer (Kim et al., 2010). These examples underscore the capacity of HTS to discover new biological activities of old drugs, often through mechanisms unrelated to their original therapeutic use.
5.6 Multi-Omics and Systems Biology
The integration of multi-omics data—spanning genomics, transcriptomics, proteomics, metabolomics, and epigenomics—has enabled a more comprehensive understanding of disease biology and drug action. Systems biology approaches analyze these data layers collectively to model the complexity of disease networks and identify actionable nodes for intervention.In the context of drug repurposing, multi-omics tools can reveal shared molecular modules across diseases and link metabolic or signaling pathways to potential therapeutic compounds. For instance, metformin, a first-line agent for type 2 diabetes, has been repurposed in oncology based on omics data implicating the AMPK-mTOR signaling axis in cancer cell metabolism and proliferation. Transcriptomic and metabolomic profiling showed that metformin suppressed tumor growth through modulation of cellular energetics and inhibition of the mTOR pathway, providing a mechanistic rationale for its repositioning in various cancers (Pollak, 2012).
These multi-omics platforms support precision repurposing, where patient-specific molecular profiles are used to predict drug efficacy and minimize off-target effects. Integrative omics tools such as iLINCS and STITCH allow researchers to match disease-specific signatures with drug-induced perturbations, creating personalized repurposing hypotheses for subpopulations with unique genetic or transcriptomic profiles.
5.7 Electronic Health Records (EHR) and Real-World Evidence
Real-world data from electronic health records (EHRs), insurance claims, and patient registries offer an additional layer of evidence for drug repurposing. These observational datasets enable researchers to identify unintended beneficial effects of medications by analyzing outcomes in large, diverse patient populations over time. When combined with advanced statistical techniques for confounding control, EHR data can reveal causal signals that warrant further clinical investigation.
For example, observational studies have reported that statin use was associated with a decreased incidence of several cancers, including colorectal and prostate cancer, prompting randomized controlled trials to explore their oncologic applications (Nielsen, Nordestgaard, & Bojesen, 2012). In another case, selective serotonin reuptake inhibitors (SSRIs), commonly used antidepressants, were observed to reduce platelet aggregation and cardiovascular risk, leading to trials assessing their utility in cardiovascular disease prevention (Wang, Wang, & Liu, 2014). Nevertheless, EHR-based repurposing studies face methodological challenges. Confounding by indication, missing data, and variability in coding practices can obscure true associations. To address these issues, methods such as propensity score matching, target trial emulation, and instrumental variable analysis have been developed to strengthen causal inference in real-world repurposing research (Hernán & Robins, 2016).
In sum, drug repurposing strategies now encompass a robust ecosystem of computational, experimental, and observational methodologies. When used in synergy, these approaches enhance the efficiency, precision, and scope of drug repositioning efforts—bringing us closer to a future where therapeutic discovery is accelerated, personalized, and guided by data.
6. Regulatory and Ethical Considerations in Drug Repurposing
While drug repurposing offers clear scientific and clinical advantages, its successful implementation depends heavily on navigating complex regulatory landscapes and ethical frameworks. Although the repurposing of approved drugs benefits from existing safety and pharmacokinetic data, these advantages do not guarantee expedited approval unless sponsors meet the requirements of regional regulatory authorities. Additionally, challenges around intellectual property (IP), commercial viability, and ethical obligations in off-label use or emergency authorization must be carefully considered. The following subsections highlight the major regulatory pathways and ethical tensions that shape the trajectory of drug repurposing in both the United States and the European Union, as well as broader issues related to intellectual property rights and global access.
6.1 Regulatory Pathways
Drug repurposing benefits from regulatory flexibility, as many repositioned agents have already undergone preclinical toxicology and early-phase human testing. However, these compounds must still pass through formal regulatory review before approval for a new indication. The pathway varies depending on the jurisdiction and the nature of the compound and its intended use.
6.1.1 United States: FDA Pathways
In the United States, the Food and Drug Administration (FDA) facilitates drug repurposing through multiple regulatory mechanisms under the Federal Food, Drug, and Cosmetic Act. One of the most relevant pathways is the 505(b)(2) New Drug Application (NDA). This hybrid regulatory pathway allows sponsors to rely on existing clinical data generated by others—often from the original approval—while submitting new data to support the new indication or formulation. This route substantially reduces the time and cost associated with clinical trials and is commonly used for repurposed drugs, particularly when the compound has an established safety profile (U.S. Food & Drug Administration, 2020).
Other notable mechanisms include the Orphan Drug Designation, which provides regulatory and financial incentives—such as tax credits, user fee waivers, and seven years of market exclusivity—for drugs repurposed to treat rare diseases. These incentives have been effective in encouraging pharmaceutical companies to pursue repositioning for niche indications (Yin, 2008). Additionally, programs like Breakthrough Therapy Designation, Fast Track, and Accelerated Approval are intended to expedite development and review of drugs for serious or life-threatening conditions. However, even with these programs, repurposing off-patent or generic drugs can be complicated by data ownership and exclusivity issues. Sponsors who do not own the original clinical data may face limitations in using it, unless they generate new bridging studies or gain access through licensing agreements.
6.1.2 European Union: EMA Guidelines
In the European Union, drug repurposing is regulated by the European Medicines Agency (EMA). One of the most applicable regulatory routes is the Well-Established Use pathway under Article 10a of Directive 2001/83/EC, which allows sponsors to submit a dossier based on bibliographic evidence rather than new clinical trial data. This pathway is particularly relevant for compounds that have been used extensively in clinical practice, and for which safety and efficacy are well-documented in the scientific literature (EMA, 2021).
To further support drug repurposing, particularly within academic institutions, the EMA has initiated pilot programs like STARS (Strengthening Training of Academia in Regulatory Science). STARS aims to provide regulatory training and support for academic researchers pursuing non-commercial drug development and repositioning projects. These initiatives reflect a growing recognition that academia plays a vital role in repurposing efforts, especially in therapeutic areas that may not be commercially attractive to large pharmaceutical companies.
6.2 Intellectual Property and Commercial Incentives
One of the most persistent barriers to drug repurposing is the issue of intellectual property protection. Many drugs that are suitable for repurposing are already off-patent or available as generics, which limits the potential for traditional market exclusivity. This lack of exclusivity can deter pharmaceutical companies from investing in repositioning efforts, as the return on investment may be compromised by generic competition (Nosengo, 2016).
To address this, sponsors may pursue various forms of secondary patents, such as use patents that protect new therapeutic indications, formulation patents that claim novel delivery systems, or combination patents that cover the use of the drug in conjunction with another therapy. However, these strategies are often insufficient to guarantee meaningful market protection, especially in the absence of data exclusivity or strong enforcement mechanisms. Academic researchers and small biotech firms face additional challenges, as they often lack the resources to navigate complex patent landscapes or fund clinical development. To overcome these barriers, public-private partnerships and philanthropic funding organizations—such as Cures Within Reach and the Global Antibiotic Research and Development Partnership (GARDP)—have emerged to support repurposing projects with limited commercial appeal. These collaborations are essential for sustaining innovation in areas like rare diseases, global health, and antimicrobial resistance, where market-driven incentives may be inadequate.

Figure 1. Overview of key repurposed drugs. The diagram illustrates the original indications, repurposed therapeutic applications, and primary mechanisms of action for thalidomide, sildenafil, metformin, and minoxidil. Arrows denote the transition from initial use to new clinical roles, highlighting how mechanistic insight enabled successful repositioning and regulatory approval or clinical progression.
6.3 Ethical Considerations
Drug repurposing also raises a number of ethical concerns, particularly when drugs are prescribed off-label or authorized under emergency use without robust clinical evidence. While off-label prescribing is legally permitted in many jurisdictions, it carries ethical risks if the safety or efficacy of the drug in the new indication is not well-established. Patients may be exposed to unforeseen side effects, drug interactions, or suboptimal treatment outcomes in the absence of appropriate oversight or informed consent (Shah, Shah, & Morganroth, 2020).
Informed consent is particularly important when repurposed drugs are used in investigational settings or under compassionate use protocols. Patients must be clearly informed that the drug is not approved for their specific condition, and that efficacy data may be limited. Transparent communication is essential to uphold patient autonomy and trust. Access and equity also represent key ethical dimensions of drug repurposing. While repositioned drugs may be less expensive due to their generic status, disparities in regulatory approval and pricing structures can limit access in low- and middle-income countries. Global repurposing strategies must account for affordability, supply chain constraints, and local health infrastructure to ensure that benefits are equitably distributed.
The COVID-19 pandemic highlighted the urgency and complexity of these ethical issues. During the early stages of the outbreak, several drugs were repurposed under Emergency Use Authorizations (EUAs)—such as remdesivir and hydroxychloroquine—based on limited clinical evidence. While EUAs can accelerate access to potentially life-saving therapies, they also carry risks of undermining public confidence, especially if subsequent trials fail to confirm efficacy (Beigel et al., 2020). Ethical frameworks must therefore balance the need for rapid action with the obligation to generate high-quality evidence and maintain scientific integrity.
In conclusion, drug repurposing operates within a multifaceted regulatory and ethical environment. While regulatory flexibility and expedited pathways offer significant advantages, challenges related to intellectual property, financial incentives, and equitable access must be addressed to fully realize the potential of drug repositioning. A coordinated, ethically grounded approach—supported by regulatory innovation, public-private collaboration, and rigorous scientific evaluation—will be essential for sustainable success in this field.
7. Success Stories in Drug Repurposing
The real-world validation of drug repurposing as a viable therapeutic strategy is best exemplified by the success stories that have transformed initially failed or narrowly scoped drugs into gold-standard treatments for entirely new indications. These examples illustrate how serendipity, clinical observation, and mechanistic insight can converge to uncover the hidden potential of existing compounds. Repurposed drugs like thalidomide, sildenafil, metformin, and minoxidil have not only overcome initial limitations but have gone on to generate significant therapeutic impact across multiple disease areas (Figure 1; Table 1). These cases also underscore the importance of mechanistic re-evaluation, long-term surveillance, and adaptive regulatory frameworks in facilitating such transitions.
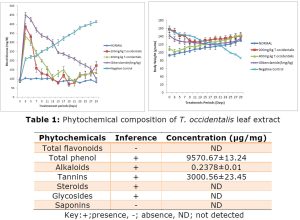
Table 1: Summary of Notable Repurposed Drugs
| Original Use | Repurposed Indication | Mechanism of Action | Status |
| Thalidomide | Multiple Myeloma, Leprosy | Immunomodulation, anti-angiogenesis | Approved |
| Sildenafil | Erectile Dysfunction, PAH | PDE5 inhibition | Approved |
| Metformin | Oncology, Aging | AMPK activation | In clinical trials |
| Disulfiram | Cancer (glioblastoma, breast) | ALDH inhibition, p97 inhibition | Phase II trials |
| Mebendazole | Brain tumors, NSCLC | Microtubule disruption | Phase I/II trials |
| Colchicine | Cardiovascular inflammation | NLRP3 inflammasome inhibition | Approved (CVD, pericarditis) |
| Itraconazole | Basal cell carcinoma | Hedgehog signaling inhibition | Off-label |
| Valproic acid | Bipolar, migraine | HDAC inhibition, GABA modulation | Approved |
| Amantadine | Parkinson’s disease | Dopamine release enhancement | Approved |
| Fluvoxamine | COVID-19, neuroinflammation | Sigma-1 receptor agonism | Emergency use/in trials |
7.1 Thalidomide
Thalidomide is perhaps the most infamous case of initial pharmaceutical failure and subsequent redemption through repurposing. Originally developed in the 1950s by Chemie Grünenthal as a sedative and treatment for morning sickness, thalidomide was rapidly withdrawn after being linked to severe teratogenic effects, including limb malformations in thousands of children worldwide (Vargesson, 2009). For decades, the drug was shunned, until its anti-inflammatory and immunomodulatory properties were rediscovered in the context of erythema nodosum leprosum (ENL), a complication of leprosy.
This pivotal finding led to its approval by the U.S. FDA in 1998 for ENL, re-establishing its therapeutic credibility. Further research revealed that thalidomide also inhibits angiogenesis and modulates cytokine production, particularly tumor necrosis factor-alpha (TNF-α), thereby making it an attractive candidate for oncology (Singhal et al., 1999). Its approval for multiple myeloma, a hematologic malignancy, marked a turning point in its clinical journey. This success catalyzed the development of structurally related but safer analogs such as lenalidomide and pomalidomide, which now form the backbone of multiple myeloma therapy (Richardson et al., 2002). Thalidomide’s journey from a teratogen to a cornerstone of modern immunomodulatory therapy highlights the complexity and potential of rational drug repurposing.
7.2 Sildenafil
Sildenafil citrate was originally synthesized by Pfizer as a treatment for angina pectoris, aiming to exploit its vasodilatory effects via inhibition of phosphodiesterase type 5 (PDE5). Although the drug failed to demonstrate sufficient efficacy in relieving anginal symptoms during early clinical trials, patients frequently reported an unexpected side effect—enhanced penile erection (Boolell et al., 1996).Recognizing the commercial and therapeutic potential of this observation, Pfizer redirected its development toward erectile dysfunction (ED). In 1998, sildenafil was approved by the FDA under the brand name Viagra, becoming the first oral medication for ED and revolutionizing sexual health management.
The drug’s mechanism of action—selective inhibition of PDE5, leading to smooth muscle relaxation and increased blood flow—also prompted its repurposing for pulmonary arterial hypertension (PAH). The pulmonary vasculature also expresses PDE5, and sildenafil’s efficacy in reducing pulmonary pressure was validated in randomized clinical trials (Galiè et al., 2005). Consequently, sildenafil was rebranded as Revatio for PAH, offering a critical therapeutic option for a rare but life-threatening condition. The dual indications of sildenafil exemplify the success of pharmacodynamic repurposing and have spurred similar strategies for other PDE5 inhibitors.
7.3 Metformin
Metformin, a biguanide class drug derived from the plant Galega officinalis, was introduced in the 1950s for the treatment of type 2 diabetes mellitus (T2DM) due to its ability to lower hepatic glucose production and improve insulin sensitivity (Rena et al., 2017). Over decades of clinical use, observational studies and mechanistic investigations began to suggest that metformin also possesses anti-proliferative, anti-inflammatory, and anti-aging effects. It activates AMP-activated protein kinase (AMPK), a key energy-sensing enzyme that regulates cell growth and metabolism. This AMPK-mediated inhibition of the mTOR pathway has positioned metformin as a promising candidate for oncology, particularly in colorectal, breast, and prostate cancers (He & Wondisford, 2015). Furthermore, metformin has demonstrated efficacy in polycystic ovary syndrome (PCOS) by ameliorating insulin resistance and restoring ovulatory cycles (Lord et al., 2003). Current clinical trials are also investigating its role in extending healthspan and reducing age-related morbidities, with the Targeting Aging with Metformin (TAME) trial representing a landmark study in geroscience (Barzilai et al., 2016). Metformin’s evolution from a humble antidiabetic agent to a multi-disease therapeutic underscores the potential of real-world evidence and mechanistic biology in driving repurposing.
7.4 Minoxidil